An Experienced Hernia Mesh Attorney
Brett Vaughn of Nigh Goldenberg Raso & Vaughn helped start many of the national hernia litigations years ago and continues to play an active role in key leadership positions. Brett drafted many of the initial hernia mesh master complaints after developing unique theories of liability for the various types of hernia mesh. On September 19, 2018, Brett Vaughn was appointed by Chief Judge Edmund A. Sargus of the Southern District of Ohio as one of six attorneys in the nation to the Bard Hernia Mesh Plaintiffs’ Executive Committee (PEC). Brett Vaughn is also the co-chair of the Bard hernia mesh science and expert committee. Brett Vaughn was also appointed by Judge John Porto in New Jersey to the Plaintiff’s Executive Committee for the Ethicon hernia mesh matters, including the Proceed, Physiomesh, and Prolene Hernia System litigations. Similarly, Brett Vaughn co-chairs the science and expert committee in the Ethicon hernia mesh litigations. Brett Vaughn also plays an active role in the Covidien hernia mesh lawsuits, though leadership positions are still pending with the court. When deciding on a hernia mesh attorney – experience matters.
Hernia Mesh is Big Business

There are many different manufacturers of hernia mesh. The main manufacturers of hernia mesh include Bard-Davol (now owned by Becton Dickinson), Covidien (now owned by Medtronic), Ethicon (owned by Johnson & Johnson), Atrium (owned by Getinge), and Gore. Hernia mesh products have extremely high profit margins (the companies make a lot of money selling hernia meshes). The largest hernia mesh manufacturer, C.R. Bard, was acquired in 2017 by Becton Dickinson for $24 billion. Companies want to protect these high-profit margins, which can result in a fierce defense and longer litigation. This current round of hernia mesh litigation started back in 2016. Fighting back against companies of this size is a long process and takes dedication. You need an attorney that is intimately involved and devoted to the hernia mesh litigations to give you the best odds.
Why Is Hernia Mesh So Profitable?
Hernia Meshes Utilize Cheap Polymers
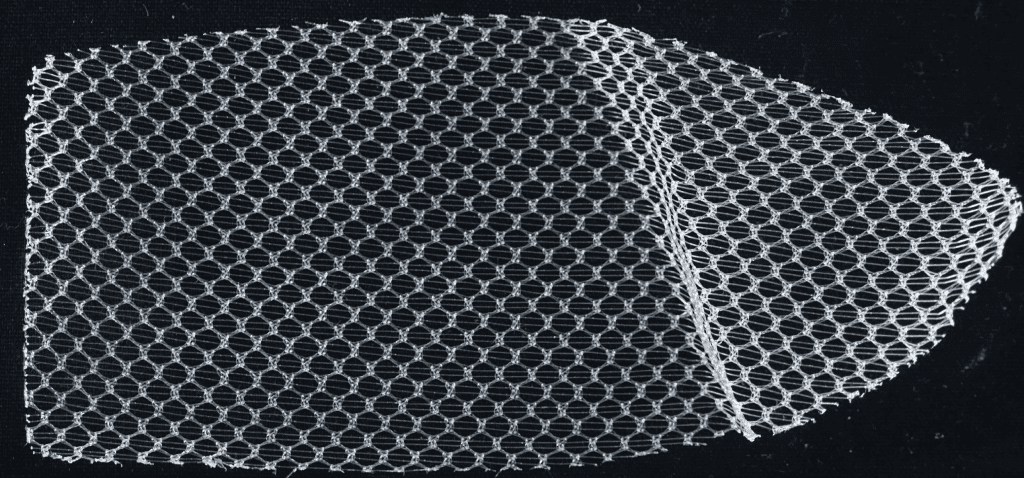
Many of these hernia mesh devices are made out of essentially petroleum waste products – like polypropylene and polyester. These cheap polymers are then made into hernia meshes and sold for hundreds to thousands of dollars per hernia mesh. Many of the polymers that hernia meshes are made of were never intended to be permanently implanted in humans.
Polypropylene – Don’t Implant in Humans!

The above medical application caution is from the polypropylene that the company Bard Davol utilizes to make most of its hernia meshes. The polypropylene is called Marlex polypropylene and is made by the company Chevron Phillips. Bard Davol was warned by Chevron Phillips Chemical Company not to use this polypropylene (plastic) for permanent human implantation over a decade ago! However, Bard continued to make hundreds of thousands of hernia mesh devices out of Marlex polypropylene. Our hernia mesh attorneys have alleged that this Marlex polypropylene is degraded before it is ever implanted in a patient. After implantation, our hernia mesh lawyers allege that the Marlex polypropylene undergoes significant degradation due to oxidation, resulting in mesh contracture and deformation.
Hernia Meshes Use Gimmick Designs to Charge More
Decades ago, hernia meshes were just flat sheets of polypropylene. When a polypropylene hernia mesh is flat it is much less dangerous, as it is at less risk of mesh deformation. However, flat sheets of polypropylene hernia mesh don’t sell for a lot of money, something like $20-$50 per mesh (still a high-profit margin when the base polymer is the same thing fishing line and tennis rackets are made out of). Hernia mesh manufacturers then started selling hernia meshes with one the following gimmicks that made the meshes more dangerous, but allowed the companies to sell the hernia meshes for several hundred to thousands of dollars per mesh:
-
Hernia Mesh Plugs
These plug hernia meshes came to the market in the early 2000’s and were intended primarily for inguinal hernia repair, but were also marketed and utilized in some ventral (abdominal wall) hernia repairs. These hernia mesh plugs were advertised to surgeons as being able to just be put into the hernia, that way the surgeon wouldn’t even have to close the hernia defect. This would allow surgeons to do their hernia procedures faster, therefore the surgeon could do more hernia procedures in a day. The hernia mesh companies could charge several hundreds of dollars for these plug type hernia meshes.

These hernia mesh plugs are a large ball of mesh (like a ball of tangled up fishing line) that are intended to incite a profound inflammatory response so that the body scars in the hernia mesh plug to the hernia defect. Unfortunately, this intense inflammatory response and uncontrolled formation of scar tissue also cause a large number of patients to experience chronic debilitating pain as a result of their nerves and other structures getting caught up in the inflammatory and scarification process. When a male patient’s spermatic cord gets caught up in this inflammatory and scarification process, it can result in an orchiectomy (removal of the testicle). The three-dimensional design of hernia mesh plugs also increases the risk that the hernia mesh will migrate or erode through surrounding tissue over time. The American Hernia Society came out several years ago and advised against the utilization of plugs in hernia repair due to the increased rates of hernia mesh migration.
-
Coating Polypropylene Hernia Meshes With Permanent ePTFE
In the early 2000’s hernia meshes started being sold that were polypropylene with a permanent ePTFE (expanded polytetrafluoroethylene) layer sewn to the polypropylene layer with polypropylene thread. The ePTFE layer of the hernia mesh is essentially like Gore-Tex which is used in a non-stick raincoat. The polypropylene of the hernia mesh will stick to any tissue it touches, and that can cause severe complications if the polypropylene sticks to a patient’s bowels or other organs. The ePTFE was added to the polypropylene for its non-stick properties. The ePTFE was to be positioned between the polypropylene and any sensitive organs. This allowed surgeons to be able to implant the hernia meshes even closer to the bowels and without as much time spent dissecting the tissue planes. Some of the polypropylene + ePTFE composite hernia meshes began selling for over $1,000.
The polypropylene + ePTFE composite meshes came with increased rates of many severe complications. The increased rates of complications and mesh failures were not communicated to patients or implanting surgeons. Rates of chronic infection with polypropylene/ePTFE composite meshes went up sharply. The profound inflammatory response from the polypropylene attracts bacteria, while the small pores of the ePTFE can harbor the bacteria. The pores of ePTFE are large enough for bacteria to enter, but too large for white blood cells. As a result, many patients have experienced infections for years, needing a wound vac and many debridements. ePTFE also contracts over time, resulting in exposure of the polypropylene to sensitive organs over time. Many patients implanted with ePTFE+polypropylene hernia meshes have experienced bowel obstructions, bowel resection, and erosion.
-
Resorbable Coated Hernia Meshes

Due to the high rates of infection with permanent ePTFE barriers, companies started to make hernia mesh barriers out of resorbable materials. These resorbable coated hernia meshes were advertised as having less permanent foreign body, thereby decreasing the risk of infection. Most of these resorbable barriers were also advertised as lasting for the duration of the critical wound healing period (which the hernia mesh manufacturers typically defined as approximately 28 days). However, many of these resorbable hernia mesh coatings resorb enough to expose bare polypropylene to the bowel and other organs within hours to days. Many patients implanted with resorbable coated hernia meshes experience abdominal complications, such bowel obstructions, stomach pains, bowel resections, bowel perforations, erosion, and infection.
-
Hernia Mesh Patches
Hernia mesh patches are either polypropylene + ePTFE composite meshes or polypropylene + resorbable coating composite meshes that are made into small circular patches. These patches have a memory recoil ring in the middle of the mesh to allow the mesh to return to its original shape after being folded up. These hernia patches also have straps that allowed the surgeon to pull the hernia patch to the abdominal wall after implantation and flatten the mesh as it is fixated. Hernia mesh patches significantly decrease the necessary skill level of the implanting surgeon. Hernia mesh patches are both quick and easy to implant.

Hernia mesh patches fail at a much higher rate than non-patch hernia mesh. Hernia mesh patches experience larger amounts of shrinkage or contraction. The degree of shrinkage that hernia mesh patches undergo results in higher rates of hernia mesh recurrence when a hernia patch it utilized. Hernia mesh patches also shrink to such a degree that they can deform the mesh – resulting in the dangerous polypropylene being exposed to sensitive organs like the bowel. Some hernia mesh patches also contain permanent memory recoil rings. As the mesh shrinks over time, too much pressure can be put on the memory ring, resulting in a ring break. Hernia mesh ring breaks have resulted in bowel perforations and even death.

Hernia mesh patches are typically for very small hernias (<3 cm). Many of these small hernias could be fixed without mesh at all – just using a suture. When hernia mesh patches fail, a much larger hernia defect results, because so much tissue has to be removed with the hernia mesh. Subsequent hernia surgeries will then be more likely to have to use hernia mesh, and a larger piece of hernia mesh. Hernia mesh patches have turned very small problems into very large problems for many patients.
-
Self-Fixating Hernia Meshes

As an answer to the high complaint rates of chronic pain associated with hernia meshes, the mesh manufacturers came up with hernia meshes that didn’t require fixation, such as using sutures or tacks to secure the mesh in place. These meshes were advertised to surgeons as resulting in lower rates of chronic pain (even though no pre-market human studies were ever conducted). Hernia meshes that don’t require surgeons to fixate the mesh in place, resulted in even quicker surgeries that even less skilled surgeons could perform.
Many complications are associated with the use of fixationless hernia meshes. Many of the hernia meshes that don’t require fixation also don’t properly incorporate into the surrounding tissue. This results in mesh migration, mesh deformation (wrinkling and folding), chronic pain, and higher rates of recurrence. Some of the hernia meshes that don’t require fixation have thousands of microhooks on one side of the mesh to help the mesh stick to the tissue like Velcro. These Velcro-like microhooks result in many patients experiencing severe, chronic, debilitating pain. To make matters worse, the hernia mesh is extremely difficult to remove because of all of the microhooks. Surgeons frequently have to “piece-meal” the mesh out, where they remove very small sections of mesh at a time – creating a very long and complicated surgery. Many patients require numerous surgeries to remove all of the mesh. Surgeons frequently are unable to remove all of the mesh, because parts of the mesh have adhered to the femoral artery, and removing it could kill the patient.

Hernia Meshes Designed So Less Experienced Surgeons Can Implant
As discussed above, all of the mesh gimmicks were created to expand the market of hernia mesh. Either by making the hernia mesh easier to implant or by permitting the mesh to be utilized in a different manner, such as closer to the bowel. A general surgeon can make significantly more money if they are doing quick, high-frequency hernia mesh repairs. However, when the cheap gimmick meshes fail, it takes a significantly more skilled surgeon to remove the failed hernia mesh and fix the resulting problems. Many patients complain that the surgeon that implanted their failed hernia mesh refuses to reoperate on them. Many hernia mesh victims have to travel great distances to find a skilled enough surgeon to reoperate on them after a hernia mesh failure.
Unfortunately, hernia mesh use has become so prevelant, that most surgical residencies only train surgeons on repairing hernias with mesh. The skill of repairing a hernia without mesh is becoming a lost art. One hospital in Ontario Canada, Shouldice Hospital, specializes in repairing inguinal hernias without the use of hernia mesh, in a procedure known as the shouldice repair. Not only are surgeons losing the ability to repair hernias without mesh, many surgeons are also losing the ability to repair hernias with a flat piece of mesh. Placing the mesh in a plane away from the bowel can take a significant amount of skill and require meticulous dissection, but results in lower complication rates. The safest hernia repairs take longer, require much more skill, and are less profitable. The incentives in the US medical industry aren’t structured around results and patient safety, they are structured around profits.
Hernia Mesh Injuries
Hernia meshes can result in a wide variety and severity of injuries depending on which mesh was utilized and where the hernia mesh was placed. Below is a list and description of mesh injuries and the types of hernia mesh they are most commonly associated with.
- Bowel Obstruction:

Patient experiences chronic abdominal and stomach pain after implantation of the hernia mesh. These symptoms can begin years after the hernia mesh was implanted. The frequency of bowel movements becomes less regular and less often. Eventually the patient is unable to have a bowel movement. This can result from the hernia mesh becoming adhered to the bowel. Hernia mesh forms dense adhesions when it becomes in contact with the bowel. Depending on how extensive and dense the bowel adhesions are, sometimes parts of the bowel have to be resected with the hernia mesh. Many patients have experienced bowel resections as a result of failed hernia meshes.
Ventral or abdominal wall hernia meshes are more commonly associated with bowel obstructions when compared to inguinal hernia meshes. The closer a hernia mesh is placed to the bowel, the higher the risk of bowel obstruction. Hernia meshes with a permanent ePTFE barrier, a resorbable barrier, and hernia mesh patches are associated with the highest rates of bowel obstruction. - Chronic Infections:

Patient experiences infections associated with the hernia mesh for months and years after implantation. Many of these mesh infections are resistant to oral and even I.V. antibiotic treatment. These chronic infections also frequently result in large non-healing wounds and wound dehiscence (wound opening back up). Many hernia mesh victims have required long-term wound vac treatment. Other hernia mesh victims have died as a result of sepsis.
Chronic hernia mesh infections occur more often in ventral or abdominal wall hernias than inguinal hernias. The closer the hernia mesh is placed to the bowel, the higher the risk of infection. Hernia meshes with permanent and resorbable barriers appear to increase the risk of infection. Hernia meshes with a permanent ePTFE barrier can harbor bacteria while preventing white blood cells from clearing an infection. Heavier-weight polypropylene also has a higher infection rate when compared to lighter-weight polypropylene. Finally, polyester, especially multi-filament polyester meshes greatly increase the risk of infection. - Chronic Debilitating Pain:
Patient is unable to continue normal activities of daily living due to pain severity. Pain medications, nerve injections, and nerve removals do not alleviate patient’s mesh pain. Due to the difficulty in treating mesh pain, many patients have been referred for psychiatric treatment. The mesh pain is real though and is frequently relieved when all of the pieces of hernia mesh have been fully removed. Sometimes it can take several months after mesh removal for the nerves to calm back down and the pain to subside.
Chronic pain can be associated with both ventral and inguinal hernias, but the highest rates of debilitating pain appear to be associated with inguinal hernia meshes. When inguinal hernia meshes change from a flat design to a three-dimensional design, rates of chronic pain increase. Plug type hernia meshes have much higher rates of chronic pain. As do self-adhering hernia meshes. - Hernia Recurrence: Patient experiences the same hernia that a mesh was previously utilized to repair. Hernia mesh is advertised heavily on being able to significantly reduce the rate of hernia recurrence. However, when a hernia does recur after mesh has been placed, the subsequent surgery is significantly more complex. The old hernia mesh typically needs to be removed, which then results in an even larger hernia that needs repaired. With an even larger hernia, many surgeons will elect to place an even larger hernia mesh. Many patients have had numerous hernia meshes fail over a decade, resulting in increasingly complex repair surgeries.
Hernia mesh patches have very high rates of hernia recurrence. Some hernia meshes were also made too weak to sustain the normal pressures of the abdominal cavity and would tear. Hernia mesh plugs and self-fixating meshes also migrate and can lead to hernia recurrence.
Hernia Mesh Failure Modes
There are many unique types of hernia meshes are the market, resulting in many unique failure modes. Some of the more commonly observed hernia mesh failure modes are listed below. Hernia meshes are sold as permanent, life-long medical implants.
- Ring Break or Buckle:
A hernia mesh ring break is associated with two types of hernia mesh – Bard’s Kugel hernia mesh and Bard’s Ventralex hernia mesh, both of which contained a permanent PET (polyethylene terephthalate) ring. Both of these hernia meshes are patches, and subject to significant shrinkage. As the hernia mesh shrinks and deforms, it puts more pressure on the ring. If enough force is applied, eventually the ring will buckle or break. If the ring buckles or breaks, the mesh deforms and can cause organ perforation. The polypropylene side of the mesh can also then be exposed to the bowel and result in dense adhesions and bowel obstruction. The risk of mesh erosion also significantly increases once the mesh deforms. Hernia mesh ring breaks and buckles result in significant hospitalizations and surgeries. There have been thousands of hernia mesh lawsuits filed that have alleged the ring broke, buckled, or folded after implantation.
- Mesh Tearing:
Some hernia meshes have high rates of tearing, rupturing, or blowing out. This is mostly due to some hernia meshes being made with materials that are not strong enough. Many hernia mesh companies attempted to reduce the amount of polypropylene as much as possible in hopes of reducing complications. However, hernia mesh complications subsequently increased due to the meshes blowing out. The hernia mesh lawsuits allege that some hernia meshes are being sterilized by gamma irradiation, which can decrease the strength of polypropylene hernia mesh. Hernia meshes tearing, rupturing, or blowing out can result in recurrences and significant bowel injuries. When a hernia mesh blows out, the bowel frequently gets entangled with the hernia mesh. The hernia mesh can also tear at the spot of fixation, resulting in the hernia mesh balling up and the hernia recurring.
- Mesh Deformation: The hernia mesh lawsuits allege that making a hernia mesh three-dimensional or adding layers to the hernia mesh increases the risk of mesh deformation. Even a small wrinkle forming in a hernia mesh after implantation can result in chronic pain. Some hernia meshes are also made of cheap plastics that degrade before and after they are implanted in the human body. These hernia meshes become weaker over time and more likely to deform. Hernia mesh deformation not only causes severe pain, but also increases the risk of mesh migration, erosion, bowel obstruction, and infection.
- Meshoma:
A meshoma is a large ball of tissue and mesh that looks like a tumor. Meshomas are frequently associated with severe chronic pain. Meshomas are usually the result of mesh deformation or mesh plugs. A wadded-up ball of mesh elicits a profound inflammatory response, resulting in a ball of scar tissue.
Hernia Mesh Settlements
There are many hernia mesh companies, each of which manufactures numerous hernia meshes that are subject to litigation. A couple of hernia mesh manufacturers have settled or are settling claims against them related to a select few hernia meshes. Most information related to any hernia mesh settlement is highly confidential and can not be discussed online or with others. However, one thing is true with all settlements of this nature – they are a lengthy process. Even after an initial hernia mesh settlement is announced, the entire settlement has to be administered. The settlement process in a hernia mesh settlement typically takes between a year to a year and a half. During this time, your claim is being submitted and argued, appealed when necessary (sometimes multiple times), and liens are being vetted and negotiated. All claims in a hernia mesh settlement have to be adjudicated so that the amount of money that each client receives can be determined. The hernia mesh lawsuits are not class actions, so the amount of money an individual receives is highly individualized based on the specific facts of their hernia mesh claim. Insurance companies also have a right to seek reimbursement for some of the treatment they paid for related to your hernia mesh injuries. During the hernia mesh settlement process, these insurance liens are significantly negotiated down, so that you retain as much of your hernia mesh settlement as possible. Sometimes hernia mesh settlements are distributed in multiple payments while insurance liens are still being vetted and negotiated. This allows the client to receive some of their hernia mesh settlement money sooner, while liens are being finalized. While some hernia mesh companies have settled, it is important to realize that doesn’t mean that other hernia mesh companies will settle or settle anytime in the near future. Our hernia mesh attorneys are prepared to continue fighting for the years to come.
Hernia Mesh Updates on Specific Hernia Mesh Manufacturers
Bard hernia mesh lawsuit updates. Learn more about the specifics of the Bard Davol hernia mesh lawsuits, including the state and federal court Bard hernia mesh litigations.
Covidien hernia mesh lawsuit updates. Learn more about the specifics of the Covidien hernia mesh lawsuits, including the state and federal court Covidien hernia mesh litigations.
Hernia Mesh Statute of Limitations
All cases are subject to various hernia mesh statutes of limitations, so contact our hernia mesh attorneys today if you think you might have been injured by a defective hernia mesh device. Contact our hernia mesh attorneys today at 202-792-7927. Acquiring all the necessary medical records to support your hernia mesh claim can take a significant amount of time to acquire. Do not wait to contact our hernia mesh attorneys if you think that you’ve been injured by hernia mesh.